Module 6: The Lymphatic and Immune Systems
Lesson 5: The Immune Response against Pathogens
Đáp Ứng Miễn Dịch Chống Lại Tác Nhân
Dưới đây là danh sách những thuật ngữ Y khoa của module The Lymphatic and Immune Systems.
Khái quát được số lượng thuật ngữ sẽ xuất hiện trong bài đọc và nghe sẽ giúp bạn thoải mái tiêu thụ nội dung hơn. Sau khi hoàn thành nội dung đọc và nghe, bạn hãy quay lại đây và luyện tập (practice) để quen dần các thuật ngữ này. Đừng ép bản thân phải nhớ các thuật ngữ này vội vì bạn sẽ gặp và ôn lại danh sách này trong những bài học (lesson) khác của cùng một module.
Medical Terminology: The Lymphatic and Immune Systems
active immunity
immunity developed from an individual’s own immune system
acute inflammation
inflammation occurring for a limited time period; rapidly developing
adaptive immune response
relatively slow but very specific and effective immune response controlled by lymphocytes
afferent lymphatic vessels
lead into a lymph node
antibody
antigen-specific protein secreted by plasma cells; immunoglobulin
antigen
molecule recognized by the receptors of B and T lymphocytes
antigen presentation
binding of processed antigen to the protein-binding cleft of a major histocompatibility complex molecule
antigen processing
internalization and digestion of antigen in an antigen-presenting cell
antigen receptor
two-chain receptor by which lymphocytes recognize antigen
antigenic determinant
(also, epitope) one of the chemical groups recognized by a single type of lymphocyte antigen receptor
B cells
lymphocytes that act by differentiating into an antibody-secreting plasma cell
barrier defenses
antipathogen defenses deriving from a barrier that physically prevents pathogens from entering the body to establish an infection
bone marrow
tissue found inside bones; the site of all blood cell differentiation and maturation of B lymphocytes
bronchus-associated lymphoid tissue (BALT)
lymphoid nodule associated with the respiratory tract
central tolerance
B cell tolerance induced in immature B cells of the bone marrow
chemokine
soluble, long-range, cell-to-cell communication molecule
chronic inflammation
inflammation occurring for long periods of time
chyle
lipid-rich lymph inside the lymphatic capillaries of the small intestine
cisterna chyli
bag-like vessel that forms the beginning of the thoracic duct
class switching
ability of B cells to change the class of antibody they produce without altering the specificity for antigen
clonal anergy
process whereby B cells that react to soluble antigens in bone marrow are made nonfunctional
clonal deletion
removal of self-reactive B cells by inducing apoptosis
clonal expansion
growth of a clone of selected lymphocytes
clonal selection
stimulating growth of lymphocytes that have specific receptors
clone
group of lymphocytes sharing the same antigen receptor
complement
enzymatic cascade of constitutive blood proteins that have antipathogen effects, including the direct killing of bacteria
constant region domain
part of a lymphocyte antigen receptor that does not vary much between different receptor types
cytokine
soluble, short-range, cell-to-cell communication molecule
cytotoxic T cells (Tc)
T lymphocytes with the ability to induce apoptosis in target cells
delayed hypersensitivity
(type IV) T cell-mediated immune response against pathogens infiltrating interstitial tissues, causing cellular infiltrate
early induced immune response
includes antimicrobial proteins stimulated during the first several days of an infection
effector T cells
immune cells with a direct, adverse effect on a pathogen
efferent lymphatic vessels
lead out of a lymph node
erythroblastosis fetalis
disease of Rh factor-positive newborns in Rh-negative mothers with multiple Rh-positive children; resulting from the action of maternal antibodies against fetal blood
fas ligand
molecule expressed on cytotoxic T cells and NK cells that binds to the fas molecule on a target cell and induces it do undergo apoptosis
Fc region
in an antibody molecule, the site where the two termini of the heavy chains come together; many cells have receptors for this portion of the antibody, adding functionality to these molecules
germinal centers
clusters of rapidly proliferating B cells found in secondary lymphoid tissues
graft-versus-host disease
in bone marrow transplants; occurs when the transplanted cells mount an immune response against the recipient
granzyme
apoptosis-inducing substance contained in granules of NK cells and cytotoxic T cells
heavy chain
larger protein chain of an antibody
helper T cells (Th)
T cells that secrete cytokines to enhance other immune responses, involved in activation of both B and T cell lymphocytes
high endothelial venules
vessels containing unique endothelial cells specialized to allow migration of lymphocytes from the blood to the lymph node
histamine
vasoactive mediator in granules of mast cells and is the primary cause of allergies and anaphylactic shock
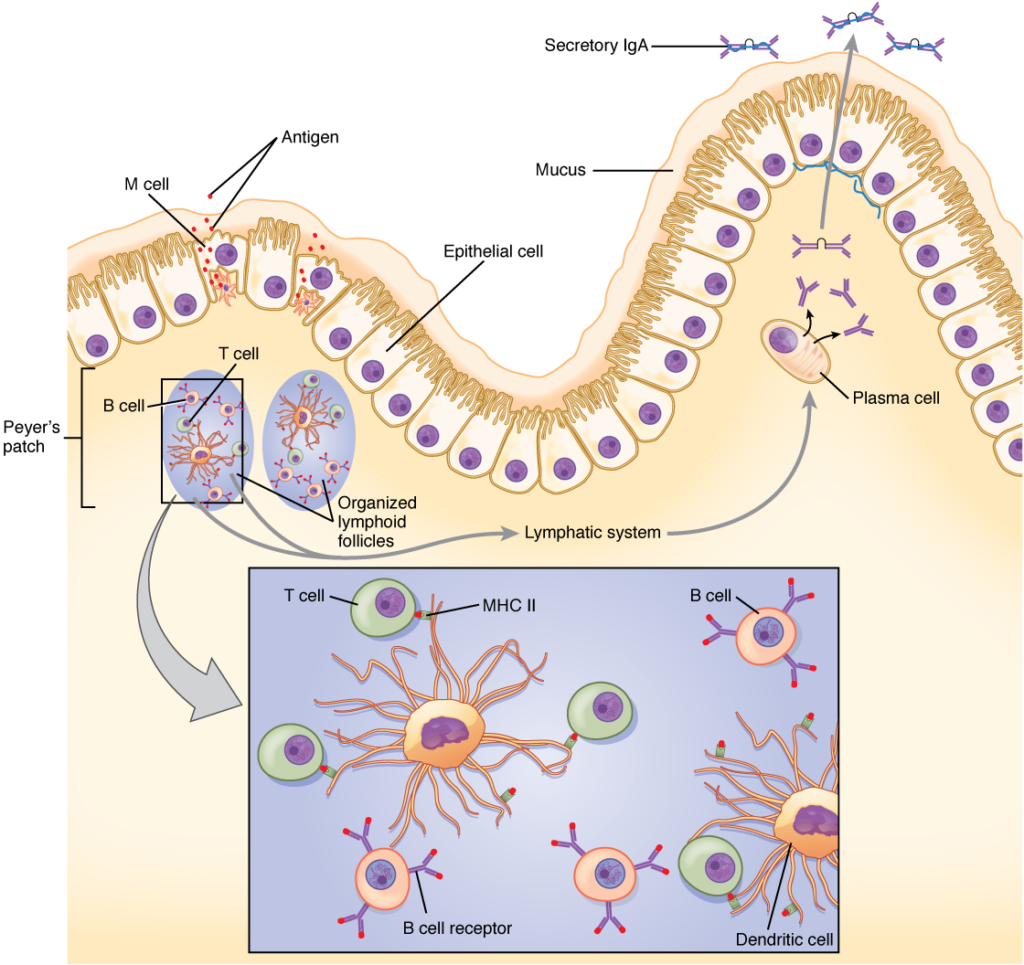
IgA
antibody whose dimer is secreted by exocrine glands, is especially effective against digestive and respiratory pathogens, and can pass immunity to an infant through breastfeeding
IgD
class of antibody whose only known function is as a receptor on naive B cells; important in B cell activation
IgE
antibody that binds to mast cells and causes antigen-specific degranulation during an allergic response
IgG
main blood antibody of late primary and early secondary responses; passed from carrier to unborn child via placenta
IgM
antibody whose monomer is a surface receptor of naive B cells; the pentamer is the first antibody made blood plasma during primary responses
immediate hypersensitivity
(type I) IgE-mediated mast cell degranulation caused by crosslinking of surface IgE by antigen
immune system
series of barriers, cells, and soluble mediators that combine to response to infections of the body with pathogenic organisms
immunoglobulin
protein antibody; occurs as one of five main classes
immunological memory
ability of the adaptive immune response to mount a stronger and faster immune response upon re-exposure to a pathogen
inflammation
basic innate immune response characterized by heat, redness, pain, and swelling
innate immune response
rapid but relatively nonspecific immune response
interferons
early induced proteins made in virally infected cells that cause nearby cells to make antiviral proteins
light chain
small protein chain of an antibody
lymph
fluid contained within the lymphatic system
lymph node
one of the bean-shaped organs found associated with the lymphatic vessels
lymphatic capillaries
smallest of the lymphatic vessels and the origin of lymph flow
lymphatic system
network of lymphatic vessels, lymph nodes, and ducts that carries lymph from the tissues and back to the bloodstream.
lymphatic trunks
large lymphatics that collect lymph from smaller lymphatic vessels and empties into the blood via lymphatic ducts
lymphocytes
white blood cells characterized by a large nucleus and small rim of cytoplasm
lymphoid nodules
unencapsulated patches of lymphoid tissue found throughout the body
macrophage
ameboid phagocyte found in several tissues throughout the body
macrophage oxidative metabolism
metabolism turned on in macrophages by T cell signals that help destroy intracellular bacteria
major histocompatibility complex (MHC)
gene cluster whose proteins present antigens to T cells
mast cell
cell found in the skin and the lining of body cells that contains cytoplasmic granules with vasoactive mediators such as histamine
memory T cells
long-lived immune cell reserved for future exposure to a pathogen
MHC class I
found on most cells of the body, it binds to the CD8 molecule on T cells
MHC class II
found on macrophages, dendritic cells, and B cells, it binds to CD4 molecules on T cells
MHC polygeny
multiple MHC genes and their proteins found in body cells
MHC polymorphism
multiple alleles for each individual MHC locus
monocyte
precursor to macrophages and dendritic cells seen in the blood
mucosa-associated lymphoid tissue (MALT)
lymphoid nodule associated with the mucosa
naïve lymphocyte
mature B or T cell that has not yet encountered antigen for the first time
natural killer cell (NK)
cytotoxic lymphocyte of innate immune response
negative selection
selection against thymocytes in the thymus that react with self-antigen
neutralization
inactivation of a virus by the binding of specific antibody
neutrophil
phagocytic white blood cell recruited from the bloodstream to the site of infection via the bloodstream
opsonization
enhancement of phagocytosis by the binding of antibody or antimicrobial protein
passive immunity
transfer of immunity to a pathogen to an individual that lacks immunity to this pathogen usually by the injection of antibodies
pattern recognition receptor (PRR)
leukocyte receptor that binds to specific cell wall components of different bacterial species
perforin
molecule in NK cell and cytotoxic T cell granules that form pores in the membrane of a target cell
peripheral tolerance
mature B cell made tolerant by lack of T cell help
phagocytosis
movement of material from the outside to the inside of the cells via vesicles made from invaginations of the plasma membrane
plasma cell
differentiated B cell that is actively secreting antibody
polyclonal response
response by multiple clones to a complex antigen with many determinants
positive selection
selection of thymocytes within the thymus that interact with self, but not non-self, MHC molecules
primary adaptive response
immune system’s response to the first exposure to a pathogen
primary lymphoid organ
site where lymphocytes mature and proliferate; red bone marrow and thymus gland
psychoneuroimmunology
study of the connections between the immune, nervous, and endocrine systems
regulatory T cells (Treg)
(also, suppressor T cells) class of CD4 T cells that regulates other T cell responses
right lymphatic duct
drains lymph fluid from the upper right side of body into the right subclavian vein
secondary adaptive response
immune response observed upon re-exposure to a pathogen, which is stronger and faster than a primary response
secondary lymphoid organs
sites where lymphocytes mount adaptive immune responses; examples include lymph nodes and spleen
sensitization
first exposure to an antigen
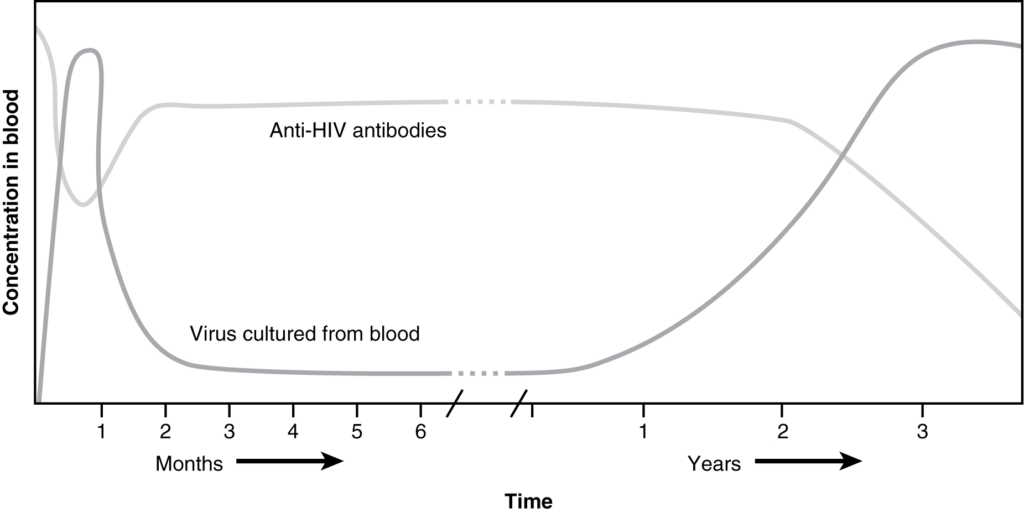
seroconversion
clearance of pathogen in the serum and the simultaneous rise of serum antibody
severe combined immunodeficiency disease (SCID)
genetic mutation that affects both T cell and B cell arms of the immune response
spleen
secondary lymphoid organ that filters pathogens from the blood (white pulp) and removes degenerating or damaged blood cells (red pulp)
T cell
lymphocyte that acts by secreting molecules that regulate the immune system or by causing the destruction of foreign cells, viruses, and cancer cells
T cell tolerance
process during T cell differentiation where most T cells that recognize antigens from one’s own body are destroyed
T cell-dependent antigen
antigen that binds to B cells, which requires signals from T cells to make antibody
T cell-independent antigen
binds to B cells, which do not require signals from T cells to make antibody
Th1 cells
cells that secrete cytokines that enhance the activity of macrophages and other cells
Th2 cells
cells that secrete cytokines that induce B cells to differentiate into antibody-secreting plasma cells
thoracic duct
large duct that drains lymph from the lower limbs, left thorax, left upper limb, and the left side of the head
thymocyte
immature T cell found in the thymus
thymus
primary lymphoid organ; where T lymphocytes proliferate and mature
tissue typing
typing of MHC molecules between a recipient and donor for use in a potential transplantation procedure
tonsils
lymphoid nodules associated with the nasopharynx
type I hypersensitivity
immediate response mediated by mast cell degranulation caused by the crosslinking of the antigen-specific IgE molecules on the mast cell surface
type II hypersensitivity
cell damage caused by the binding of antibody and the activation of complement, usually against red blood cells
type III hypersensitivity
damage to tissues caused by the deposition of antibody-antigen (immune) complexes followed by the activation of complement
variable region domain
part of a lymphocyte antigen receptor that varies considerably between different receptor types
Dưới đây là các bài văn nằm ở bên trái. Ở bên phải là các bài luyện tập (practice) để đánh giá khả năng đọc hiểu của bạn. Sẽ khó khăn trong thời gian đầu nếu vốn từ vựng của bạn còn hạn chế, đặc biệt là từ vựng Y khoa. Hãy kiên nhẫn và đọc nhiều nhất có kể, lượng kiến thức tích tụ dần sẽ giúp bạn đọc thoải mái hơn.
Dưới đây là video và các luyện tập (practice) của bài này. Nghe là một kĩ năng khó, đặc biệt là khi chúng ta chưa quen nội dung và chưa có nhạy cảm ngôn ngữ. Nhưng cứ đi thật chậm và đừng bỏ cuộc.
Dưới đây là phần bàn luận. Bạn có thể tự do đặt câu hỏi, bổ sung kiến thức, và chia sẻ trải nghiệm của mình.
Subscribe
Login
0 Comments
Ấn vào ô bên dưới để đánh dấu bạn đã hoàn thành bài học này
Quá dữ! Tiếp tục duy trì phong độ nhé!