Module 11: The Neurological Exam
Lesson 5: The Coordination and Gait Exams
Khám Phối Hợp Vận Động Và Dáng Đi
Dưới đây là danh sách những thuật ngữ Y khoa của module The Neurological Exam.
Khái quát được số lượng thuật ngữ sẽ xuất hiện trong bài đọc và nghe sẽ giúp bạn thoải mái tiêu thụ nội dung hơn. Sau khi hoàn thành nội dung đọc và nghe, bạn hãy quay lại đây và luyện tập (practice) để quen dần các thuật ngữ này. Đừng ép bản thân phải nhớ các thuật ngữ này vội vì bạn sẽ gặp và ôn lại danh sách này trong những bài học (lesson) khác của cùng một module.
Medical Terminology: The Neurological Exam
accommodation
in vision, a change in the ability of the eye to focus on objects at different distances
accommodation–convergence reflex
coordination of somatic control of the medial rectus muscles of either eye with the parasympathetic control of the ciliary bodies to maintain focus while the eyes converge on visual stimuli near to the face
anterograde amnesia
inability to form new memories from a particular time forward
aphasia
loss of language function
ataxia
movement disorder related to damage of the cerebellum characterized by loss of coordination in voluntary movements
Babinski sign
dorsiflexion of the foot with extension and splaying of the toes in response to the plantar reflex, normally suppressed by corticospinal input
cerebrocerebellum
lateral regions of the cerebellum; named for the significant input from the cerebral cortex
check reflex
response to a release in resistance so that the contractions stop, or check, movement
clasp-knife response
sign of UMN disease when a patient initially resists passive movement of a muscle but will quickly release to a lower state of resistance
conduction aphasia
loss of language function related to connecting the understanding of speech with the production of speech, without either specific function being lost
conductive hearing
hearing dependent on the conduction of vibrations of the tympanic membrane through the ossicles of the middle ear
conjugate gaze
coordinated movement of the two eyes simultaneously in the same direction
convergence
in vision, the movement of the eyes so that they are both pointed at the same point in space, which increases for stimuli that are closer to the subject
coordination exam
major section of the neurological exam that assesses complex, coordinated motor functions of the cerebellum and associated motor pathways
cortico-ponto-cerebellar pathway
projection from the cerebral cortex to the cerebellum by way of the gray matter of the pons
cranial nerve exam
major section of the neurological exam that assesses sensory and motor functions of the cranial nerves and their associated central and peripheral structures
cytoarchitecture
study of a tissue based on the structure and organization of its cellular components; related to the broader term, histology
deep tendon reflex
another term for stretch reflex, based on the elicitation through deep stimulation of the tendon at the insertion
diplopia
double vision resulting from a failure in conjugate gaze
edema
fluid accumulation in tissue; often associated with circulatory deficits
embolus
obstruction in a blood vessel such as a blood clot, fatty mass, air bubble, or other foreign matter that interrupts the flow of blood to an organ or some part of the body
episodic memory
memory of specific events in an autobiographical sense
expressive aphasia
loss of the ability to produce language; usually associated with damage to Broca’s area in the frontal lobe
extrinsic muscles of the tongue
muscles that are connected to other structures, such as the hyoid bone or the mandible, and control the position of the tongue
fasciculation
small muscle twitch as a result of spontaneous activity from an LMN
fauces
opening from the oral cavity into the pharynx
fibrillation
in motor responses, a spontaneous muscle action potential that occurs in the absence of neuromuscular input, resulting from LMN lesions
flaccid paralysis
loss of voluntary muscle control and muscle tone, as the result of LMN disease
flaccidity
presentation of a loss of muscle tone, observed as floppy limbs or a lack of resistance to passive movement
flocculonodular lobe
lobe of the cerebellum that receives input from the vestibular system to help with balance and posture
gait
rhythmic pattern of alternating movements of the lower limbs during locomotion
gait exam
major section of the neurological exam that assesses the cerebellum and descending pathways in the spinal cord through the coordinated motor functions of walking; a portion of the coordination exam
gnosis
in a neurological exam, intuitive experiential knowledge tested by interacting with common objects or symbols
graphesthesia
perception of symbols, such as letters or numbers, traced in the palm of the hand
hemisection
cut through half of a structure, such as the spinal cord
hemorrhagic stroke
disruption of blood flow to the brain caused by bleeding within the cranial vault
hyperflexia
overly flexed joints
hypotonicity
low muscle tone, a sign of LMN disease
hypovolemia
decrease in blood volume
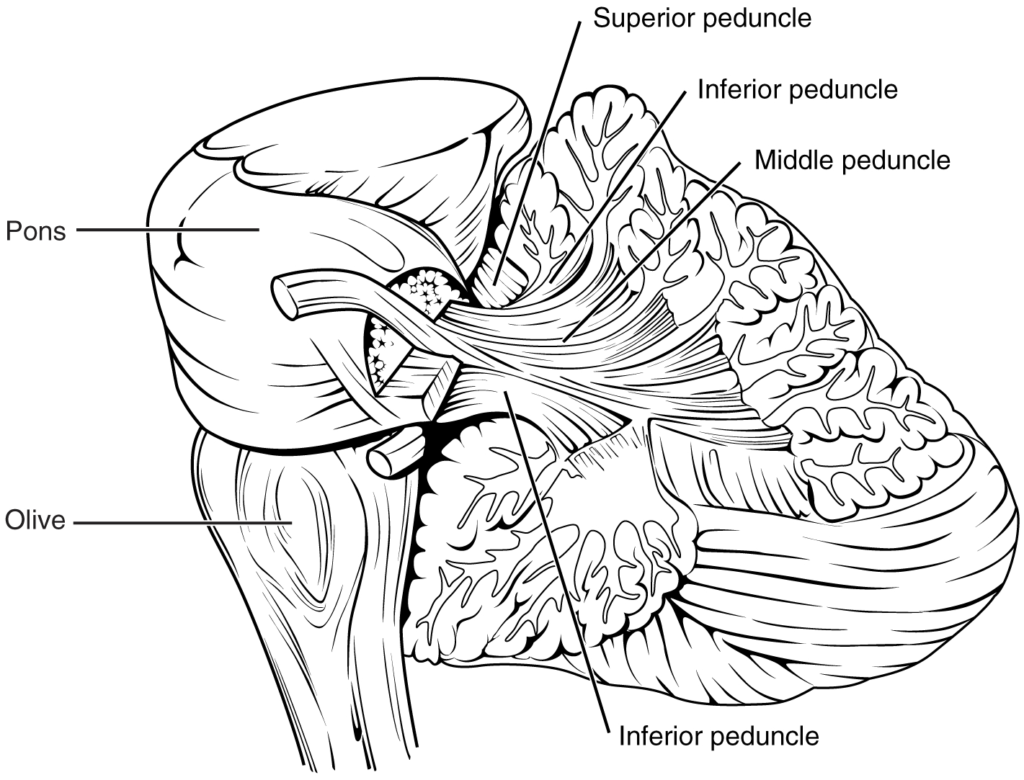
inferior cerebellar peduncle (ICP)
input to the cerebellum, largely from the inferior olive, that represents sensory feedback from the periphery
inferior olive
large nucleus in the medulla that receives input from sensory systems and projects into the cerebellar cortex
internuclear ophthalmoplegia
deficit of conjugate lateral gaze because the lateral rectus muscle of one eye does not contract resulting from damage to the abducens nerve or the MLF
intorsion
medial rotation of the eye around its axis
intrinsic muscles of the tongue
muscles that originate out of, and insert into, other tissues within the tongue and control the shape of the tongue
ischemic stroke
disruption of blood flow to the brain because blood cannot flow through blood vessels as a result of a blockage or narrowing of the vessel
jaw-jerk reflex
stretch reflex of the masseter muscle
localization of function
principle that circumscribed anatomical locations are responsible for specific functions in an organ system
medial longitudinal fasciculus (MLF)
fiber pathway that connects structures involved in the control of eye and head position, from the superior colliculus to the vestibular nuclei and cerebellum
mental status exam
major section of the neurological exam that assesses cognitive functions of the cerebrum
middle cerebellar peduncle (MCP)
large, white-matter bridge from the pons that constitutes the major input to the cerebellar cortex
motor exam
major section of the neurological exam that assesses motor functions of the spinal cord and spinal nerves
neurological exam
clinical assessment tool that can be used to quickly evaluate neurological function and determine if specific parts of the nervous system have been affected by damage or disease
paramedian pontine reticular formation (PPRF)
region of the brain stem adjacent to the motor nuclei for gaze control that coordinates rapid, conjugate eye movements
paresis
partial loss of, or impaired, voluntary muscle control
plantar reflex
superficial reflex initiated by gentle stimulation of the sole of the foot
praxis
in a neurological exam, the act of doing something using ready knowledge or skills in response to verbal instruction
procedural memory
memory of how to perform a specific task
pronator drift
sign of contralateral corticospinal lesion when the one arm will drift into a pronated position when held straight out with the palms facing upward
receptive aphasia
loss of the ability to understand received language, such as what is spoken to the subject or given in written form
red nucleus
nucleus in the midbrain that receives output from the cerebellum and projects onto the spinal cord in the rubrospinal tract
retrograde amnesia
loss of memories before a particular event
Rinne test
use of a tuning fork to test conductive hearing loss versus sensorineural hearing loss
Romberg test
test of equilibrium that requires the patient to maintain a straight, upright posture without visual feedback of position
rubrospinal tract
descending tract from the red nucleus of the midbrain that results in modification of ongoing motor programs
saccade
small, rapid movement of the eyes used to locate and direct the fovea onto visual stimuli
sensorineural hearing
hearing dependent on the transduction and propagation of auditory information through the neural components of the peripheral auditory structures
sensory exam
major section of the neurological exam that assesses sensory functions of the spinal cord and spinal nerves
short-term memory
capacity to retain information actively in the brain for a brief period of time
Snellen chart
standardized arrangement of letters in decreasing size presented to a subject at a distance of 20 feet to test visual acuity
spasticity
increased contraction of a muscle in response to resistance, often resulting in hyperflexia
spinocerebellar tract
ascending fibers that carry proprioceptive input to the cerebellum used in maintaining balance and coordinated movement
spinocerebellum
midline region of the cerebellum known as the vermis that receives proprioceptive input from the spinal cord
stereognosis
perception of common objects placed in the hand solely on the basis of manipulation of that object in the hand
stroke
(also, cerebrovascular accident (CVA)) loss of neurological function caused by an interruption of blood flow to a region of the central nervous system
superficial reflex
reflexive contraction initiated by gentle stimulation of the skin
superior cerebellar peduncle (SCP)
white-matter tract representing output of the cerebellum to the red nucleus of the midbrain
transient ischemic attack (TIA)
temporary disruption of blood flow to the brain in which symptoms occur rapidly but last only a short time
vermis
prominent ridge along the midline of the cerebellum that is referred to as the spinocerebellum
vestibulo-ocular reflex (VOR)
reflex based on connections between the vestibular system and the cranial nerves of eye movements that ensures that images are stabilized on the retina as the head and body move
vestibulocerebellum
flocculonodular lobe of the cerebellum named for the vestibular input from the eighth cranial nerve
Weber test
use of a tuning fork to test the laterality of hearing loss by placing it at several locations on the midline of the skull
Wernicke’s area
region at the posterior end of the lateral sulcus in which speech comprehension is localized
Dưới đây là các bài văn nằm ở bên trái. Ở bên phải là các bài luyện tập (practice) để đánh giá khả năng đọc hiểu của bạn. Sẽ khó khăn trong thời gian đầu nếu vốn từ vựng của bạn còn hạn chế, đặc biệt là từ vựng Y khoa. Hãy kiên nhẫn và đọc nhiều nhất có kể, lượng kiến thức tích tụ dần sẽ giúp bạn đọc thoải mái hơn.
Dưới đây là video và các luyện tập (practice) của bài này. Nghe là một kĩ năng khó, đặc biệt là khi chúng ta chưa quen nội dung và chưa có nhạy cảm ngôn ngữ. Nhưng cứ đi thật chậm và đừng bỏ cuộc.
Dưới đây là phần bàn luận. Bạn có thể tự do đặt câu hỏi, bổ sung kiến thức, và chia sẻ trải nghiệm của mình.
Subscribe
Login
0 Comments
Ấn vào ô bên dưới để đánh dấu bạn đã hoàn thành bài học này
Quá dữ! Tiếp tục duy trì phong độ nhé!