Module 28: Development and Inheritance
Lesson 4: Physiological Changes in Pregnancy
Thay Đổi Sinh Lý Trong Thai Kỳ
Dưới đây là danh sách những thuật ngữ Y khoa của module Development and Inheritance.
Khái quát được số lượng thuật ngữ sẽ xuất hiện trong bài đọc và nghe sẽ giúp bạn thoải mái tiêu thụ nội dung hơn. Sau khi hoàn thành nội dung đọc và nghe, bạn hãy quay lại đây và luyện tập (practice) để quen dần các thuật ngữ này. Đừng ép bản thân phải nhớ các thuật ngữ này vội vì bạn sẽ gặp và ôn lại danh sách này trong những bài học (lesson) khác của cùng một module.
Medical Terminology: Development and Inheritance
acrosomal reaction
release of digestive enzymes by sperm that enables them to burrow through the corona radiata and penetrate the zona pellucida of an oocyte prior to fertilization
acrosome
cap-like vesicle located at the anterior-most region of a sperm that is rich with lysosomal enzymes capable of digesting the protective layers surrounding the oocyte
afterbirth
third stage of childbirth in which the placenta and associated fetal membranes are expelled
allantois
finger-like outpocketing of yolk sac forms the primitive excretory duct of the embryo; precursor to the urinary bladder
allele
alternative forms of a gene that occupy a specific locus on a specific gene
amnion
transparent membranous sac that encloses the developing fetus and fills with amniotic fluid
amniotic cavity
cavity that opens up between the inner cell mass and the trophoblast; develops into amnion
autosomal chromosome
in humans, the 22 pairs of chromosomes that are not the sex chromosomes (XX or XY)
autosomal dominant
pattern of dominant inheritance that corresponds to a gene on one of the 22 autosomal chromosomes
autosomal recessive
pattern of recessive inheritance that corresponds to a gene on one of the 22 autosomal chromosomes
blastocoel
fluid-filled cavity of the blastocyst
blastocyst
term for the conceptus at the developmental stage that consists of about 100 cells shaped into an inner cell mass that is fated to become the embryo and an outer trophoblast that is fated to become the associated fetal membranes and placenta
blastomere
daughter cell of a cleavage
Braxton Hicks contractions
weak and irregular peristaltic contractions that can occur in the second and third trimesters; they do not indicate that childbirth is imminent
brown adipose tissue
highly vascularized fat tissue that is packed with mitochondria; these properties confer the ability to oxidize fatty acids to generate heat
capacitation
process that occurs in the female reproductive tract in which sperm are prepared for fertilization; leads to increased motility and changes in their outer membrane that improve their ability to release enzymes capable of digesting an oocyte’s outer layers
carrier
heterozygous individual who does not display symptoms of a recessive genetic disorder but can transmit the disorder to their offspring
chorion
membrane that develops from the syncytiotrophoblast, cytotrophoblast, and mesoderm; surrounds the embryo and forms the fetal portion of the placenta through the chorionic villi
chorionic membrane
precursor to the chorion; forms from extra-embryonic mesoderm cells
chorionic villi
projections of the chorionic membrane that burrow into the endometrium and develop into the placenta
cleavage
form of mitotic cell division in which the cell divides but the total volume remains unchanged; this process serves to produce smaller and smaller cells
codominance
pattern of inheritance that corresponds to the equal, distinct, and simultaneous expression of two different alleles
colostrum
thick, yellowish substance secreted from a mother’s breasts in the first postpartum days; rich in immunoglobulins
conceptus
pre-implantation stage of a fertilized egg and its associated membranes
corona radiata
in an oocyte, a layer of granulosa cells that surrounds the oocyte and that must be penetrated by sperm before fertilization can occur
cortical reaction
following fertilization, the release of cortical granules from the oocyte’s plasma membrane into the zona pellucida creating a fertilization membrane that prevents any further attachment or penetration of sperm; part of the slow block to polyspermy
dilation
first stage of childbirth, involving an increase in cervical diameter
dominant
describes a trait that is expressed both in homozygous and heterozygous form
dominant lethal
inheritance pattern in which individuals with one or two copies of a lethal allele do not survive in utero or have a shortened life span
ductus arteriosus
shunt in the pulmonary trunk that diverts oxygenated blood back to the aorta
ductus venosus
shunt that causes oxygenated blood to bypass the fetal liver on its way to the inferior vena cava
ectoderm
primary germ layer that develops into the central and peripheral nervous systems, sensory organs, epidermis, hair, and nails
ectopic pregnancy
implantation of an embryo outside of the uterus
embryo
developing human during weeks 3–8
embryonic folding
process by which an embryo develops from a flat disc of cells to a three-dimensional shape resembling a cylinder
endoderm
primary germ layer that goes on to form the gastrointestinal tract, liver, pancreas, and lungs
epiblast
upper layer of cells of the embryonic disc that forms from the inner cell mass; gives rise to all three germ layers
episiotomy
incision made in the posterior vaginal wall and perineum that facilitates vaginal birth
expulsion
second stage of childbirth, during which the mother bears down with contractions; this stage ends in birth
fertilization
unification of genetic material from male and female haploid gametes
fertilization membrane
impenetrable barrier that coats a nascent zygote; part of the slow block to polyspermy
fetus
developing human during the time from the end of the embryonic period (week 9) to birth
foramen ovale
shunt that directly connects the right and left atria and helps divert oxygenated blood from the fetal pulmonary circuit
foremilk
watery, translucent breast milk that is secreted first during a feeding and is rich in lactose and protein; quenches the infant’s thirst
gastrulation
process of cell migration and differentiation into three primary germ layers following cleavage and implantation
genotype
complete genetic makeup of an individual
gestation
in human development, the period required for embryonic and fetal development in utero; pregnancy
heterozygous
having two different alleles for a given gene
hindmilk
opaque, creamy breast milk delivered toward the end of a feeding; rich in fat; satisfies the infant’s appetite
homozygous
having two identical alleles for a given gene
human chorionic gonadotropin (hCG)
hormone that directs the corpus luteum to survive, enlarge, and continue producing progesterone and estrogen to suppress menses and secure an environment suitable for the developing embryo
hypoblast
lower layer of cells of the embryonic disc that extend into the blastocoel to form the yolk sac
implantation
process by which a blastocyst embeds itself in the uterine endometrium
incomplete dominance
pattern of inheritance in which a heterozygous genotype expresses a phenotype intermediate between dominant and recessive phenotypes
inner cell mass
cluster of cells within the blastocyst that is fated to become the embryo
involution
postpartum shrinkage of the uterus back to its pre-pregnancy volume
karyotype
systematic arrangement of images of chromosomes into homologous pairs
lactation
process by which milk is synthesized and secreted from the mammary glands of the postpartum female breast in response to sucking at the nipple
lanugo
silk-like hairs that coat the fetus; shed later in fetal development
let-down reflex
release of milk from the alveoli triggered by infant suckling
lightening
descent of the fetus lower into the pelvis in late pregnancy; also called “dropping”
lochia
postpartum vaginal discharge that begins as blood and ends as a whitish discharge; the end of lochia signals that the site of placental attachment has healed
meconium
fetal wastes consisting of ingested amniotic fluid, cellular debris, mucus, and bile
mesoderm
primary germ layer that becomes the skeleton, muscles, connective tissue, heart, blood vessels, and kidneys
morula
tightly packed sphere of blastomeres that has reached the uterus but has not yet implanted itself
mutation
change in the nucleotide sequence of DNA
neural fold
elevated edge of the neural groove
neural plate
thickened layer of neuroepithelium that runs longitudinally along the dorsal surface of an embryo and gives rise to nervous system tissue
neural tube
precursor to structures of the central nervous system, formed by the invagination and separation of neuroepithelium
neurulation
embryonic process that establishes the central nervous system
nonshivering thermogenesis
process of breaking down brown adipose tissue to produce heat in the absence of a shivering response
notochord
rod-shaped, mesoderm-derived structure that provides support for growing fetus
organogenesis
development of the rudimentary structures of all of an embryo’s organs from the germ layers
parturition
childbirth
phenotype
physical or biochemical manifestation of the genotype; expression of the alleles
placenta
organ that forms during pregnancy to nourish the developing fetus; also regulates waste and gas exchange between mother and fetus
placenta previa
low placement of fetus within uterus causes placenta to partially or completely cover the opening of the cervix as it grows
placentation
formation of the placenta; complete by weeks 14–16 of pregnancy
polyspermy
penetration of an oocyte by more than one sperm
primitive streak
indentation along the dorsal surface of the epiblast through which cells migrate to form the endoderm and mesoderm during gastrulation
prolactin
pituitary hormone that establishes and maintains the supply of breast milk; also important for the mobilization of maternal micronutrients for breast milk
Punnett square
grid used to display all possible combinations of alleles transmitted by parents to offspring and predict the mathematical probability of offspring inheriting a given genotype
quickening
fetal movements that are strong enough to be felt by the mother
recessive
describes a trait that is only expressed in homozygous form and is masked in heterozygous form
recessive lethal
inheritance pattern in which individuals with two copies of a lethal allele do not survive in utero or have a shortened life span
sex chromosomes
pair of chromosomes involved in sex determination; in males, the XY chromosomes; in females, the XX chromosomes
shunt
circulatory shortcut that diverts the flow of blood from one region to another
somite
one of the paired, repeating blocks of tissue located on either side of the notochord in the early embryo
syncytiotrophoblast
superficial cells of the trophoblast that fuse to form a multinucleated body that digests endometrial cells to firmly secure the blastocyst to the uterine wall
trait
variation of an expressed characteristic
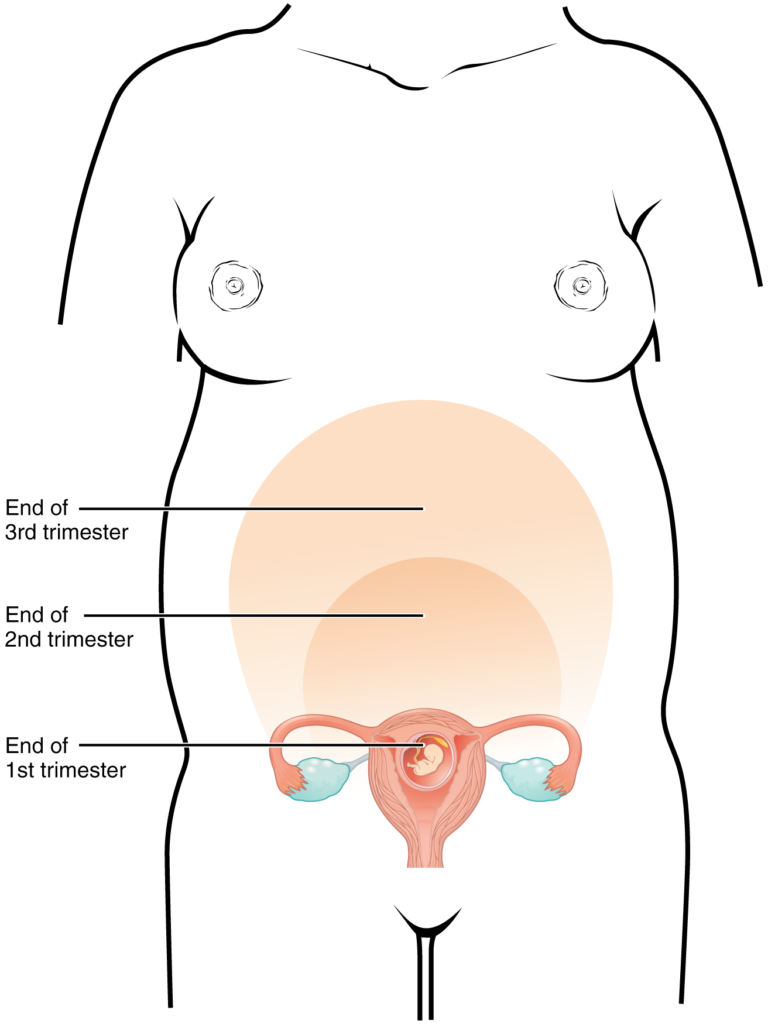
trimester
division of the duration of a pregnancy into three 3-month terms
trophoblast
fluid-filled shell of squamous cells destined to become the chorionic villi, placenta, and associated fetal membranes
true labor
regular contractions that immediately precede childbirth; they do not abate with hydration or rest, and they become more frequent and powerful with time
umbilical cord
connection between the developing conceptus and the placenta; carries deoxygenated blood and wastes from the fetus and returns nutrients and oxygen from the mother
vernix caseosa
waxy, cheese-like substance that protects the delicate fetal skin until birth
X-linked
pattern of inheritance in which an allele is carried on the X chromosome of the 23rd pair
X-linked dominant
pattern of dominant inheritance that corresponds to a gene on the X chromosome of the 23rd pair
X-linked recessive
pattern of recessive inheritance that corresponds to a gene on the X chromosome of the 23rd pair
yolk sac
membrane associated with primitive circulation to the developing embryo; source of the first blood cells and germ cells and contributes to the umbilical cord structure
zona pellucida
thick, gel-like glycoprotein membrane that coats the oocyte and must be penetrated by sperm before fertilization can occur
zygote
fertilized egg; a diploid cell resulting from the fertilization of haploid gametes from the male and female lines
Dưới đây là các bài văn nằm ở bên trái. Ở bên phải là các bài luyện tập (practice) để đánh giá khả năng đọc hiểu của bạn. Sẽ khó khăn trong thời gian đầu nếu vốn từ vựng của bạn còn hạn chế, đặc biệt là từ vựng Y khoa. Hãy kiên nhẫn và đọc nhiều nhất có kể, lượng kiến thức tích tụ dần sẽ giúp bạn đọc thoải mái hơn.
Dưới đây là video và các luyện tập (practice) của bài này. Nghe là một kĩ năng khó, đặc biệt là khi chúng ta chưa quen nội dung và chưa có nhạy cảm ngôn ngữ. Nhưng cứ đi thật chậm và đừng bỏ cuộc.
Dưới đây là phần bàn luận. Bạn có thể tự do đặt câu hỏi, bổ sung kiến thức, và chia sẻ trải nghiệm của mình.
Subscribe
Login
0 Comments
Ấn vào ô bên dưới để đánh dấu bạn đã hoàn thành bài học này
Quá dữ! Tiếp tục duy trì phong độ nhé!