Dưới đây là danh sách những thuật ngữ Y khoa của module The Urinary System.
Khái quát được số lượng thuật ngữ sẽ xuất hiện trong bài đọc và nghe sẽ giúp bạn thoải mái tiêu thụ nội dung hơn. Sau khi hoàn thành nội dung đọc và nghe, bạn hãy quay lại đây và luyện tập (practice) để quen dần các thuật ngữ này. Đừng ép bản thân phải nhớ các thuật ngữ này vội vì bạn sẽ gặp và ôn lại danh sách này trong những bài học (lesson) khác của cùng một module.
Medical Terminology: The Urinary System
anatomical sphincter
smooth or skeletal muscle surrounding the lumen of a vessel or hollow organ that can restrict flow when contracted
angiotensin I
protein produced by the enzymatic action of renin on angiotensinogen; inactive precursor of angiotensin II
angiotensin II
protein produced by the enzymatic action of ACE on inactive angiotensin I; actively causes vasoconstriction and stimulates aldosterone release by the adrenal cortex
angiotensin-converting enzyme (ACE)
enzyme produced by the lungs that catalyzes the reaction of inactive angiotensin I into active angiotensin II
angiotensinogen
inactive protein in the circulation produced by the liver; precursor of angiotensin I; must be modified by the enzymes renin and ACE to be activated
anuria
absence of urine produced; production of 50 mL or less per day
aquaporin
protein-forming water channels through the lipid bilayer of the cell; allows water to cross; activation in the collecting ducts is under the control of ADH
Bowman’s capsule
cup-shaped sack lined by a simple squamous epithelium (parietal surface) and specialized cells called podocytes (visceral surface) that participate in the filtration process; receives the filtrate which then passes on to the PCTs
brush border
formed by microvilli on the surface of certain cuboidal cells; in the kidney it is found in the PCT; increases surface area for absorption in the kidney
calyces
cup-like structures receiving urine from the collecting ducts where it passes on to the renal pelvis and ureter
cortical nephrons
nephrons with loops of Henle that do not extend into the renal medulla
countercurrent multiplier system
involves the descending and ascending loops of Henle directing forming urine in opposing directions to create a concentration gradient when combined with variable permeability and sodium pumping
detrusor muscle
smooth muscle in the bladder wall; fibers run in all directions to reduce the size of the organ when emptying it of urine
distal convoluted tubules
portions of the nephron distal to the loop of Henle that receive hyposmotic filtrate from the loop of Henle and empty into collecting ducts
diuretic
compound that increases urine output, leading to decreased water conservation
efferent arteriole
arteriole carrying blood from the glomerulus to the capillary beds around the convoluted tubules and loop of Henle; portion of the portal system
endothelins
group of vasoconstrictive, 21-amino acid peptides; produced by endothelial cells of the renal blood vessels, mesangial cells, and cells of the DCT
external urinary sphincter
skeletal muscle; must be relaxed consciously to void urine
fenestrations
small windows through a cell, allowing rapid filtration based on size; formed in such a way as to allow substances to cross through a cell without mixing with cell contents
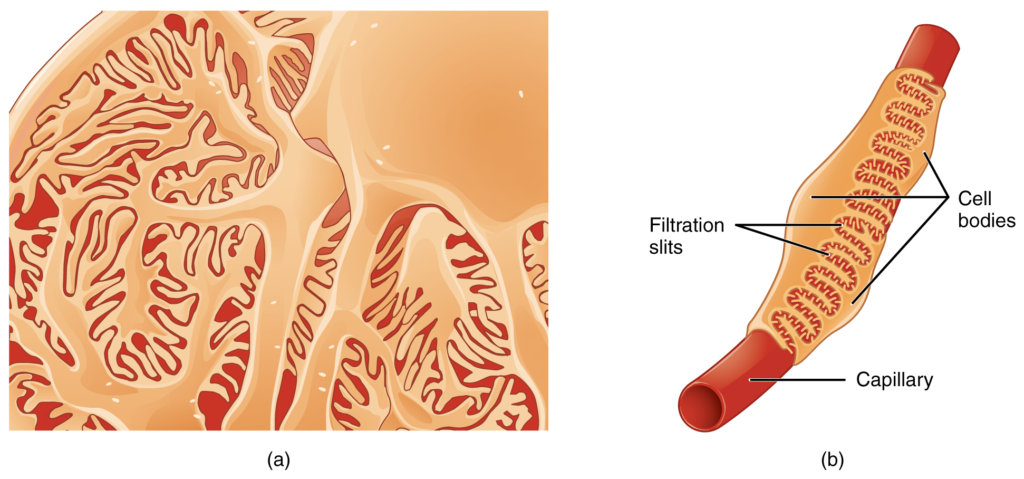
filtration slits
formed by pedicels of podocytes; substances filter between the pedicels based on size
forming urine
filtrate undergoing modifications through secretion and reabsorption before true urine is produced
glomerular filtration rate (GFR)
rate of renal filtration
glomerulus
tuft of capillaries surrounded by Bowman’s capsule; filters the blood based on size
glycosuria
presence of glucose in the urine; caused by high blood glucose levels that exceed the ability of the kidneys to reabsorb the glucose; usually the result of untreated or poorly controlled diabetes mellitus
incontinence
loss of ability to control micturition
intercalated cell
specialized cell of the collecting ducts that secrete or absorb acid or bicarbonate; important in acid–base balance
internal urinary sphincter
smooth muscle at the juncture of the bladder and urethra; relaxes as the bladder fills to allow urine into the urethra
inulin
plant polysaccharide injected to determine GFR; is neither secreted nor absorbed by the kidney, so its appearance in the urine is directly proportional to its filtration rate
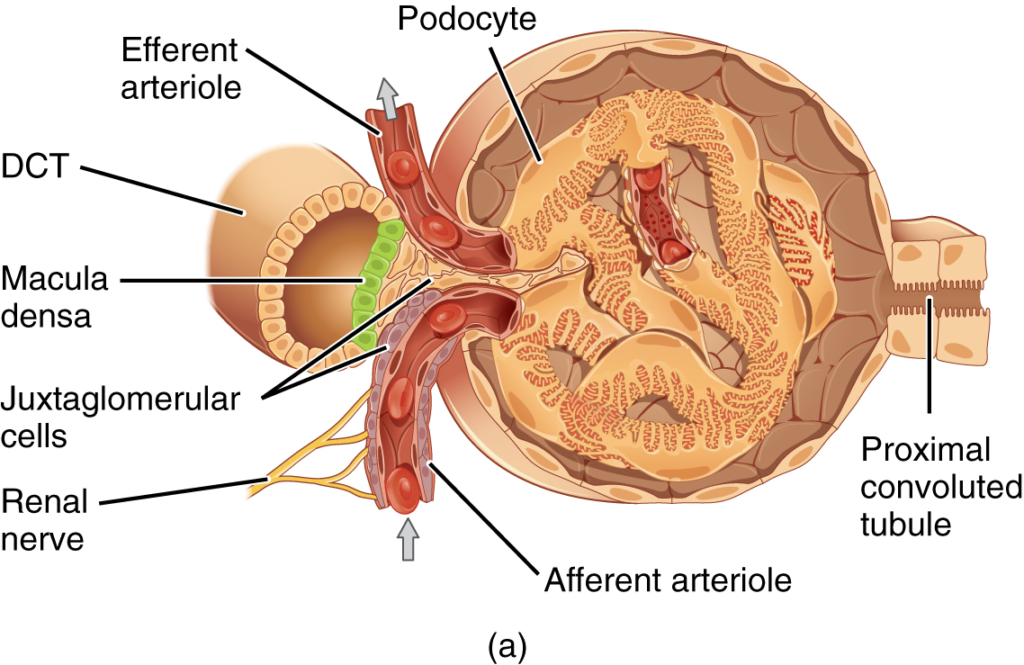
juxtaglomerular apparatus (JGA)
located at the juncture of the DCT and the afferent and efferent arterioles of the glomerulus; plays a role in the regulation of renal blood flow and GFR
juxtaglomerular cell
modified smooth muscle cells of the afferent arteriole; secretes renin in response to a drop in blood pressure
juxtamedullary nephrons
nephrons adjacent to the border of the cortex and medulla with loops of Henle that extend into the renal medulla
leaky tight junctions
tight junctions in which the sealing strands of proteins between the membranes of adjacent cells are fewer in number and incomplete; allows limited intercellular movement of solvent and solutes
leukocyte esterase
enzyme produced by leukocytes that can be detected in the urine and that serves as an indirect indicator of urinary tract infection
loop of Henle
descending and ascending portions between the proximal and distal convoluted tubules; those of cortical nephrons do not extend into the medulla, whereas those of juxtamedullary nephrons do extend into the medulla
macula densa
cells found in the part of the DCT forming the JGA; sense Na+ concentration in the forming urine
medulla
inner region of kidney containing the renal pyramids
mesangial
contractile cells found in the glomerulus; can contract or relax to regulate filtration rate
micturition
also called urination or voiding
myogenic mechanism
mechanism by which smooth muscle responds to stretch by contracting; an increase in blood pressure causes vasoconstriction and a decrease in blood pressure causes vasodilation so that blood flow downstream remains steady
nephrons
functional units of the kidney that carry out all filtration and modification to produce urine; consist of renal corpuscles, proximal and distal convoluted tubules, and descending and ascending loops of Henle; drain into collecting ducts
net filtration pressure (NFP)
pressure of fluid across the glomerulus; calculated by taking the hydrostatic pressure of the capillary and subtracting the colloid osmotic pressure of the blood and the hydrostatic pressure of Bowman’s capsule
oliguria
below normal urine production of 400–500 mL/day
osteomalacia
softening of bones due to a lack of mineralization with calcium and phosphate; most often due to lack of vitamin D; in children, osteomalacia is termed rickets; not to be confused with osteoporosis
pedicels
finger-like projections of podocytes surrounding glomerular capillaries; interdigitate to form a filtration membrane
peritubular capillaries
second capillary bed of the renal portal system; surround the proximal and distal convoluted tubules; associated with the vasa recta
physiological sphincter
sphincter consisting of circular smooth muscle indistinguishable from adjacent muscle but possessing differential innervations, permitting its function as a sphincter; structurally weak
podocytes
cells forming finger-like processes; form the visceral layer of Bowman’s capsule; pedicels of the podocytes interdigitate to form a filtration membrane
polyuria
urine production in excess of 2.5 L/day; may be caused by diabetes insipidus, diabetes mellitus, or excessive use of diuretics
principal cell
found in collecting ducts and possess channels for the recovery or loss of sodium and potassium; under the control of aldosterone; also have aquaporin channels under ADH control to regulate recovery of water
proximal convoluted tubules (PCTs)
tortuous tubules receiving filtrate from Bowman’s capsule; most active part of the nephron in reabsorption and secretion
renal columns
extensions of the renal cortex into the renal medulla; separates the renal pyramids; contains blood vessels and connective tissues
renal corpuscle
consists of the glomerulus and Bowman’s capsule
renal cortex
outer part of kidney containing all of the nephrons; some nephrons have loops of Henle extending into the medulla
renal fat pad
adipose tissue between the renal fascia and the renal capsule that provides protective cushioning to the kidney
renal hilum
recessed medial area of the kidney through which the renal artery, renal vein, ureters, lymphatics, and nerves pass
renal papillae
medullary area of the renal pyramids where collecting ducts empty urine into the minor calyces
renal pyramids
six to eight cone-shaped tissues in the medulla of the kidney containing collecting ducts and the loops of Henle of juxtamedullary nephrons
renin
enzyme produced by juxtaglomerular cells in response to decreased blood pressure or sympathetic nervous activity; catalyzes the conversion of angiotensinogen into angiotensin I
retroperitoneal
behind the peritoneum; in the case of the kidney and ureters, between the parietal peritoneum and the abdominal wall
sacral micturition center
group of neurons in the sacral region of the spinal cord that controls urination; acts reflexively unless its action is modified by higher brain centers to allow voluntary urination
specific gravity
weight of a liquid compared to pure water, which has a specific gravity of 1.0; any solute added to water will increase its specific gravity
systemic edema
increased fluid retention in the interstitial spaces and cells of the body; can be seen as swelling over large areas of the body, particularly the lower extremities
trigone
area at the base of the bladder marked by the two ureters in the posterior–lateral aspect and the urethral orifice in the anterior aspect oriented like points on a triangle
tubuloglomerular feedback
feedback mechanism involving the JGA; macula densa cells monitor Na+ concentration in the terminal portion of the ascending loop of Henle and act to cause vasoconstriction or vasodilation of afferent and efferent arterioles to alter GFR
urethra
transports urine from the bladder to the outside environment
urinalysis
analysis of urine to diagnose disease
urochrome
heme-derived pigment that imparts the typical yellow color of urine
vasa recta
branches of the efferent arterioles that parallel the course of the loops of Henle and are continuous with the peritubular capillaries; with the glomerulus, form a portal system
Dưới đây là các bài văn nằm ở bên trái. Ở bên phải là các bài luyện tập (practice) để đánh giá khả năng đọc hiểu của bạn. Sẽ khó khăn trong thời gian đầu nếu vốn từ vựng của bạn còn hạn chế, đặc biệt là từ vựng Y khoa. Hãy kiên nhẫn và đọc nhiều nhất có kể, lượng kiến thức tích tụ dần sẽ giúp bạn đọc thoải mái hơn.
Dưới đây là video và các luyện tập (practice) của bài này. Nghe là một kĩ năng khó, đặc biệt là khi chúng ta chưa quen nội dung và chưa có nhạy cảm ngôn ngữ. Nhưng cứ đi thật chậm và đừng bỏ cuộc.
Dưới đây là phần bàn luận. Bạn có thể tự do đặt câu hỏi, bổ sung kiến thức, và chia sẻ trải nghiệm của mình.
Subscribe
Login
0 Comments
Ấn vào ô bên dưới để đánh dấu bạn đã hoàn thành bài học này
Quá dữ! Tiếp tục duy trì phong độ nhé!