Dưới đây là danh sách những thuật ngữ Y khoa của module Joints.
Khái quát được số lượng thuật ngữ sẽ xuất hiện trong bài đọc và nghe sẽ giúp bạn thoải mái tiêu thụ nội dung hơn. Sau khi hoàn thành nội dung đọc và nghe, bạn hãy quay lại đây và luyện tập (practice) để quen dần các thuật ngữ này. Đừng ép bản thân phải nhớ các thuật ngữ này vội vì bạn sẽ gặp và ôn lại danh sách này trong những bài học (lesson) khác của cùng một module.
Medical Terminology: Joints
abduction
movement in the coronal plane that moves a limb laterally away from the body; spreading of the fingers
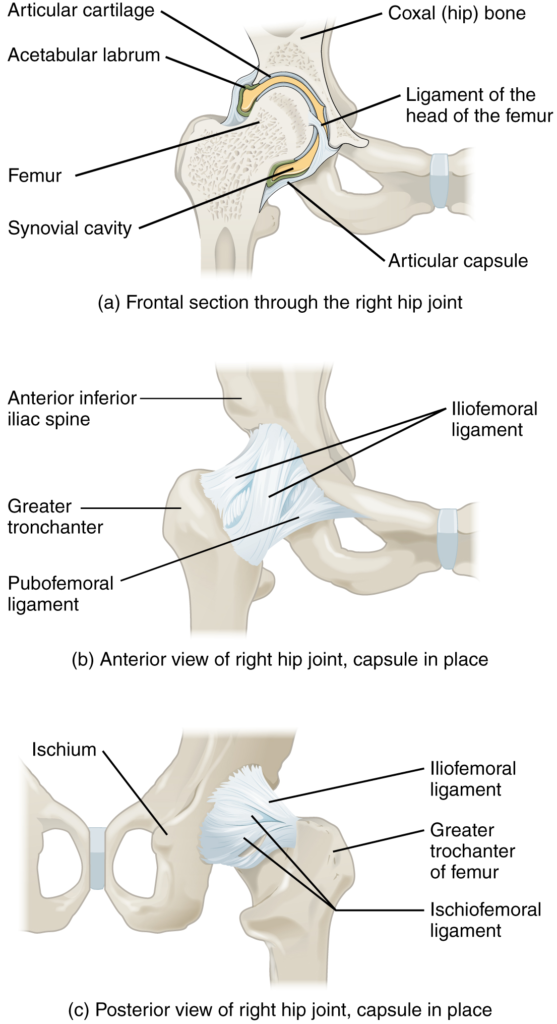
acetabular labrum
lip of fibrocartilage that surrounds outer margin of the acetabulum on the hip bone
adduction
movement in the coronal plane that moves a limb medially toward or across the midline of the body; bringing fingers together
amphiarthrosis
slightly mobile joint
annular ligament
intrinsic ligament of the elbow articular capsule that surrounds and supports the head of the radius at the proximal radioulnar joint
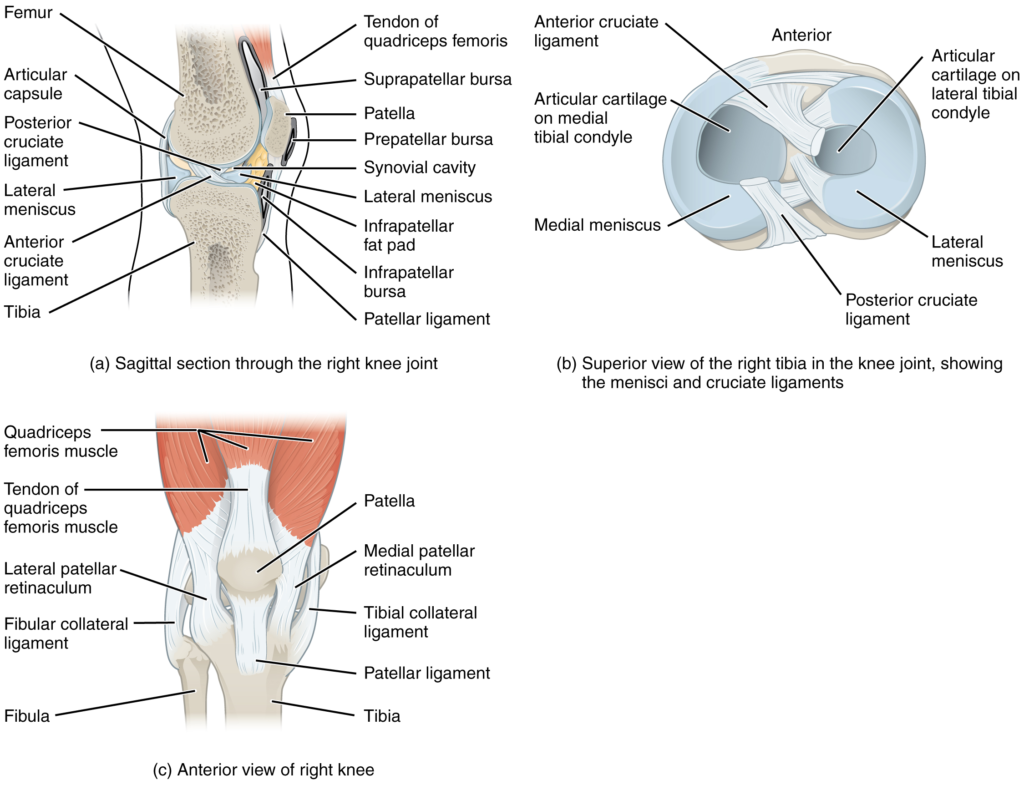
anterior cruciate ligament
intracapsular ligament of the knee; extends from anterior, superior surface of the tibia to the inner aspect of the lateral condyle of the femur; resists hyperextension of knee
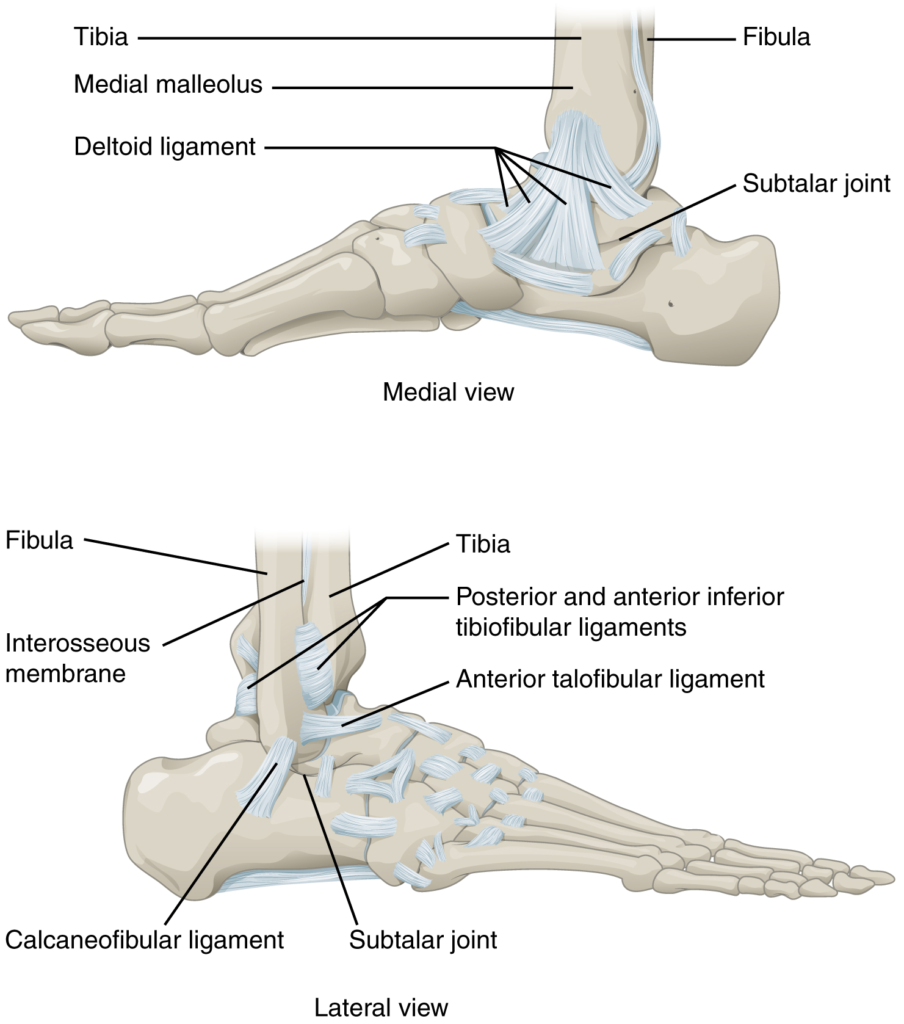
anterior talofibular ligament
intrinsic ligament located on the lateral side of the ankle joint, between talus bone and lateral malleolus of fibula; supports talus at the talocrural joint and resists excess inversion of the foot
articular capsule
connective tissue structure that encloses the joint cavity of a synovial joint
articular cartilage
thin layer of hyaline cartilage that covers the articulating surfaces of bones at a synovial joint
articular disc
meniscus; a fibrocartilage structure found between the bones of some synovial joints; provides padding or smooths movements between the bones; strongly unites the bones together
articulation
joint of the body
atlanto-occipital joint
articulation between the occipital condyles of the skull and the superior articular processes of the atlas (C1 vertebra)
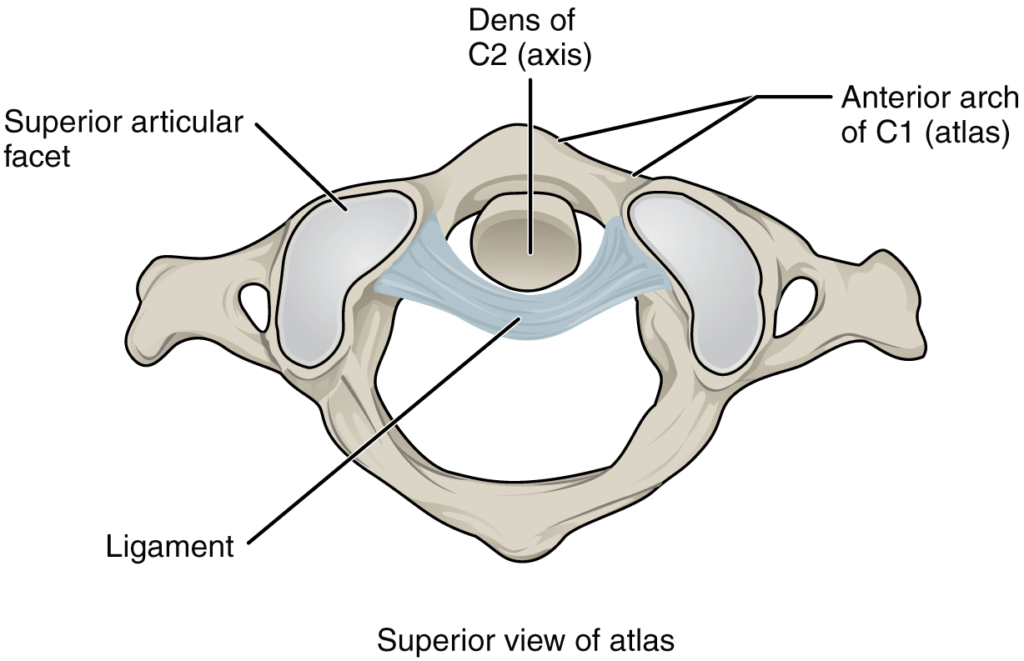
atlantoaxial joint
series of three articulations between the atlas (C1) vertebra and the axis (C2) vertebra, consisting of the joints between the inferior articular processes of C1 and the superior articular processes of C2, and the articulation between the dens of C2 and the anterior arch of C1
ball-and-socket joint
synovial joint formed between the spherical end of one bone (the ball) that fits into the depression of a second bone (the socket); found at the hip and shoulder joints; functionally classified as a multiaxial joint
biaxial joint
type of diarthrosis; a joint that allows for movements within two planes (two axes)
bursa
connective tissue sac containing lubricating fluid that prevents friction between adjacent structures, such as skin and bone, tendons and bone, or between muscles
calcaneofibular ligament
intrinsic ligament located on the lateral side of the ankle joint, between the calcaneus bone and lateral malleolus of the fibula; supports the talus bone at the ankle joint and resists excess inversion of the foot
cartilaginous joint
joint at which the bones are united by hyaline cartilage (synchondrosis) or fibrocartilage (symphysis)
circumduction
circular motion of the arm, thigh, hand, thumb, or finger that is produced by the sequential combination of flexion, abduction, extension, and adduction
condyloid joint
synovial joint in which the shallow depression at the end of one bone receives a rounded end from a second bone or a rounded structure formed by two bones; found at the metacarpophalangeal joints of the fingers or the radiocarpal joint of the wrist; functionally classified as a biaxial joint
coracohumeral ligament
intrinsic ligament of the shoulder joint; runs from the coracoid process of the scapula to the anterior humerus
deltoid ligament
broad intrinsic ligament located on the medial side of the ankle joint; supports the talus at the talocrural joint and resists excess eversion of the foot
depression
downward (inferior) motion of the scapula or mandible
diarthrosis
freely mobile joint
dorsiflexion
movement at the ankle that brings the top of the foot toward the anterior leg
elbow joint
humeroulnar joint
elevation
upward (superior) motion of the scapula or mandible
eversion
foot movement involving the intertarsal joints of the foot in which the bottom of the foot is turned laterally, away from the midline
extension
movement in the sagittal plane that increases the angle of a joint (straightens the joint); motion involving posterior bending of the vertebral column or returning to the upright position from a flexed position
extrinsic ligament
ligament located outside of the articular capsule of a synovial joint
femoropatellar joint
portion of the knee joint consisting of the articulation between the distal femur and the patella
fibrous joint
joint where the articulating areas of the adjacent bones are connected by fibrous connective tissue
fibular collateral ligament
extrinsic ligament of the knee joint that spans from the lateral epicondyle of the femur to the head of the fibula; resists hyperextension and rotation of the extended knee
flexion
movement in the sagittal plane that decreases the angle of a joint (bends the joint); motion involving anterior bending of the vertebral column
fontanelles
expanded areas of fibrous connective tissue that separate the braincase bones of the skull prior to birth and during the first year after birth
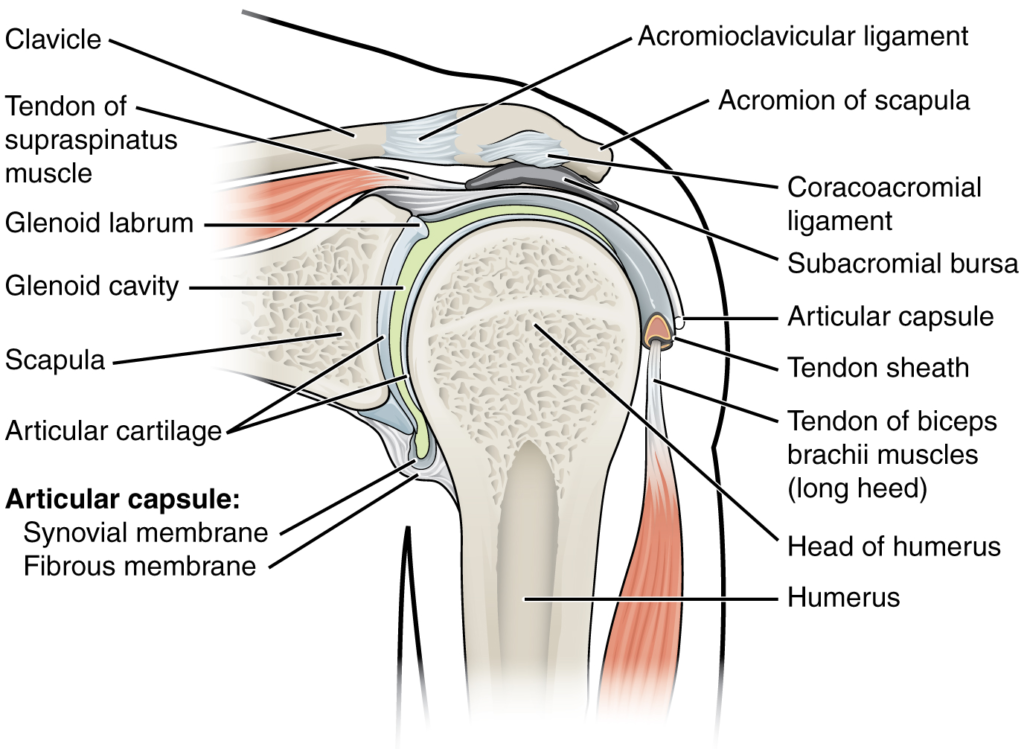
glenohumeral joint
shoulder joint; articulation between the glenoid cavity of the scapula and head of the humerus; multiaxial ball-and-socket joint that allows for flexion/extension, abduction/adduction, circumduction, and medial/lateral rotation of the humerus
glenohumeral ligament
one of the three intrinsic ligaments of the shoulder joint that strengthen the anterior articular capsule
glenoid labrum
lip of fibrocartilage located around the outside margin of the glenoid cavity of the scapula
gomphosis
type of fibrous joint in which the root of a tooth is anchored into its bony jaw socket by strong periodontal ligaments
hinge joint
synovial joint at which the convex surface of one bone articulates with the concave surface of a second bone; includes the elbow, knee, ankle, and interphalangeal joints; functionally classified as a uniaxial joint
humeroradial joint
articulation between the capitulum of the humerus and head of the radius
humeroulnar joint
articulation between the trochlea of humerus and the trochlear notch of the ulna; uniaxial hinge joint that allows for flexion/extension of the forearm
hyperextension
excessive extension of joint, beyond the normal range of movement
hyperflexion
excessive flexion of joint, beyond the normal range of movement
iliofemoral ligament
intrinsic ligament spanning from the ilium of the hip bone to the femur, on the superior-anterior aspect of the hip joint
inferior rotation
movement of the scapula during upper limb adduction in which the glenoid cavity of the scapula moves in a downward direction as the medial end of the scapular spine moves in an upward direction
interosseous membrane
wide sheet of fibrous connective tissue that fills the gap between two parallel bones, forming a syndesmosis; found between the radius and ulna of the forearm and between the tibia and fibula of the leg
intracapsular ligament
ligament that is located within the articular capsule of a synovial joint
intrinsic ligament
ligament that is fused to or incorporated into the wall of the articular capsule of a synovial joint
inversion
foot movement involving the intertarsal joints of the foot in which the bottom of the foot is turned toward the midline
ischiofemoral ligament
intrinsic ligament spanning from the ischium of the hip bone to the femur, on the posterior aspect of the hip joint
joint
site at which two or more bones or bone and cartilage come together (articulate)
joint cavity
space enclosed by the articular capsule of a synovial joint that is filled with synovial fluid and contains the articulating surfaces of the adjacent bones
joint interzone
site within a growing embryonic limb bud that will become a synovial joint
lateral (external) rotation
movement of the arm at the shoulder joint or the thigh at the hip joint that moves the anterior surface of the limb away from the midline of the body
lateral excursion
side-to-side movement of the mandible away from the midline, toward either the right or left side
lateral flexion
bending of the neck or body toward the right or left side
lateral meniscus
C-shaped fibrocartilage articular disc located at the knee, between the lateral condyle of the femur and the lateral condyle of the tibia
lateral tibiofemoral joint
portion of the knee consisting of the articulation between the lateral condyle of the tibia and the lateral condyle of the femur; allows for flexion/extension at the knee
ligament
strong band of dense connective tissue spanning between bones
ligament of the head of the femur
intracapsular ligament that runs from the acetabulum of the hip bone to the head of the femur
medial (internal) rotation
movement of the arm at the shoulder joint or the thigh at the hip joint that brings the anterior surface of the limb toward the midline of the body
medial excursion
side-to-side movement that returns the mandible to the midline
medial meniscus
C-shaped fibrocartilage articular disc located at the knee, between the medial condyle of the femur and medial condyle of the tibia
medial tibiofemoral joint
portion of the knee consisting of the articulation between the medial condyle of the tibia and the medial condyle of the femur; allows for flexion/extension at the knee
meniscus
articular disc
multiaxial joint
type of diarthrosis; a joint that allows for movements within three planes (three axes)
opposition
thumb movement that brings the tip of the thumb in contact with the tip of a finger
patellar ligament
ligament spanning from the patella to the anterior tibia; serves as the final attachment for the quadriceps femoris muscle
periodontal ligament
band of dense connective tissue that anchors the root of a tooth into the bony jaw socket
pivot joint
synovial joint at which the rounded portion of a bone rotates within a ring formed by a ligament and an articulating bone; functionally classified as uniaxial joint
plane joint
synovial joint formed between the flattened articulating surfaces of adjacent bones; functionally classified as a multiaxial joint
plantar flexion
foot movement at the ankle in which the heel is lifted off of the ground
posterior cruciate ligament
intracapsular ligament of the knee; extends from the posterior, superior surface of the tibia to the inner aspect of the medial condyle of the femur; prevents anterior displacement of the femur when the knee is flexed and weight bearing
posterior talofibular ligament
intrinsic ligament located on the lateral side of the ankle joint, between the talus bone and lateral malleolus of the fibula; supports the talus at the talocrural joint and resists excess inversion of the foot
pronated position
forearm position in which the palm faces backward
pronation
forearm motion that moves the palm of the hand from the palm forward to the palm backward position
protraction
anterior motion of the scapula or mandible
proximal radioulnar joint
articulation between head of radius and radial notch of ulna; uniaxial pivot joint that allows for rotation of radius during pronation/supination of forearm
pubofemoral ligament
intrinsic ligament spanning from the pubis of the hip bone to the femur, on the anterior-inferior aspect of the hip joint
radial collateral ligament
intrinsic ligament on the lateral side of the elbow joint; runs from the lateral epicondyle of humerus to merge with the annular ligament
reposition
movement of the thumb from opposition back to the anatomical position (next to index finger)
retraction
posterior motion of the scapula or mandible
rotation
movement of a bone around a central axis (atlantoaxial joint) or around its long axis (proximal radioulnar joint; shoulder or hip joint); twisting of the vertebral column resulting from the summation of small motions between adjacent vertebrae
rotator cuff
strong connective tissue structure formed by the fusion of four rotator cuff muscle tendons to the articular capsule of the shoulder joint; surrounds and supports superior, anterior, lateral, and posterior sides of the humeral head
saddle joint
synovial joint in which the articulating ends of both bones are convex and concave in shape, such as at the first carpometacarpal joint at the base of the thumb; functionally classified as a biaxial joint
subacromial bursa
bursa that protects the supraspinatus muscle tendon and superior end of the humerus from rubbing against the acromion of the scapula
subcutaneous bursa
bursa that prevents friction between skin and an underlying bone
submuscular bursa
bursa that prevents friction between bone and a muscle or between adjacent muscles
subscapular bursa
bursa that prevents rubbing of the subscapularis muscle tendon against the scapula
subtalar joint
articulation between the talus and calcaneus bones of the foot; allows motions that contribute to inversion/eversion of the foot
subtendinous bursa
bursa that prevents friction between bone and a muscle tendon
superior rotation
movement of the scapula during upper limb abduction in which the glenoid cavity of the scapula moves in an upward direction as the medial end of the scapular spine moves in a downward direction
supinated position
forearm position in which the palm faces anteriorly (anatomical position)
supination
forearm motion that moves the palm of the hand from the palm backward to the palm forward position
suture
fibrous joint that connects the bones of the skull (except the mandible); an immobile joint (synarthrosis)
symphysis
type of cartilaginous joint where the bones are joined by fibrocartilage
synarthrosis
immobile or nearly immobile joint
synchondrosis
type of cartilaginous joint where the bones are joined by hyaline cartilage
syndesmosis
type of fibrous joint in which two separated, parallel bones are connected by an interosseous membrane
synostosis
site at which adjacent bones or bony components have fused together
synovial fluid
thick, lubricating fluid that fills the interior of a synovial joint
synovial joint
joint at which the articulating surfaces of the bones are located within a joint cavity formed by an articular capsule
synovial membrane
thin layer that lines the inner surface of the joint cavity at a synovial joint; produces the synovial fluid
talocrural joint
ankle joint; articulation between the talus bone of the foot and medial malleolus of the tibia, distal tibia, and lateral malleolus of the fibula; a uniaxial hinge joint that allows only for dorsiflexion and plantar flexion of the foot
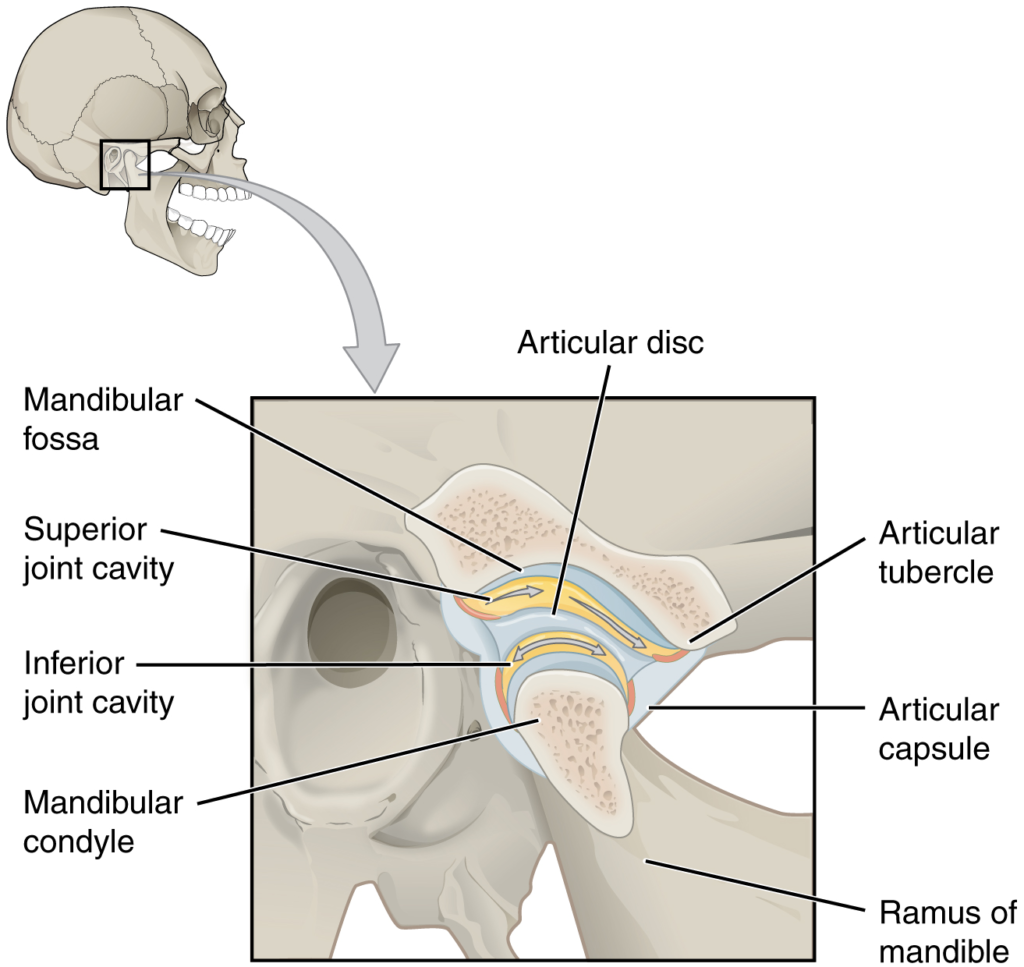
temporomandibular joint (TMJ)
articulation between the condyle of the mandible and the mandibular fossa and articular tubercle of the temporal bone of the skull; allows for depression/elevation (opening/closing of mouth), protraction/retraction, and side-to-side motions of the mandible
tendon
dense connective tissue structure that anchors a muscle to bone
tendon sheath
connective tissue that surrounds a tendon at places where the tendon crosses a joint; contains a lubricating fluid to prevent friction and allow smooth movements of the tendon
tibial collateral ligament
extrinsic ligament of knee joint that spans from the medial epicondyle of the femur to the medial tibia; resists hyperextension and rotation of extended knee
ulnar collateral ligament
intrinsic ligament on the medial side of the elbow joint; spans from the medial epicondyle of the humerus to the medial ulna
uniaxial joint
type of diarthrosis; joint that allows for motion within only one plane (one axis)
zygapophysial joints
facet joints; plane joints between the superior and inferior articular processes of adjacent vertebrae that provide for only limited motions between the vertebrae
Dưới đây là các bài văn nằm ở bên trái. Ở bên phải là các bài luyện tập (practice) để đánh giá khả năng đọc hiểu của bạn. Sẽ khó khăn trong thời gian đầu nếu vốn từ vựng của bạn còn hạn chế, đặc biệt là từ vựng Y khoa. Hãy kiên nhẫn và đọc nhiều nhất có kể, lượng kiến thức tích tụ dần sẽ giúp bạn đọc thoải mái hơn.
Dưới đây là video và các luyện tập (practice) của bài này. Nghe là một kĩ năng khó, đặc biệt là khi chúng ta chưa quen nội dung và chưa có nhạy cảm ngôn ngữ. Nhưng cứ đi thật chậm và đừng bỏ cuộc.
Dưới đây là phần bàn luận. Bạn có thể tự do đặt câu hỏi, bổ sung kiến thức, và chia sẻ trải nghiệm của mình.
Subscribe
Login
0 Comments
Ấn vào ô bên dưới để đánh dấu bạn đã hoàn thành bài học này
Quá dữ! Tiếp tục duy trì phong độ nhé!