Module 18: The Digestive System
Lesson 7: Accessory Organs in Digestion: The Liver, Pancreas, and Gallbladder
Cơ Quan Hỗ Trợ Tiêu Hóa: Gan, Tụy, Và Túi Mật
Dưới đây là danh sách những thuật ngữ Y khoa của module The Digestive System.
Khái quát được số lượng thuật ngữ sẽ xuất hiện trong bài đọc và nghe sẽ giúp bạn thoải mái tiêu thụ nội dung hơn. Sau khi hoàn thành nội dung đọc và nghe, bạn hãy quay lại đây và luyện tập (practice) để quen dần các thuật ngữ này. Đừng ép bản thân phải nhớ các thuật ngữ này vội vì bạn sẽ gặp và ôn lại danh sách này trong những bài học (lesson) khác của cùng một module.
Medical Terminology: The Digestive System
absorption
passage of digested products from the intestinal lumen through mucosal cells and into the bloodstream or lacteals
accessory digestive organ
includes teeth, tongue, salivary glands, gallbladder, liver, and pancreas
accessory duct
(also, duct of Santorini) duct that runs from the pancreas into the duodenum
acinus
cluster of glandular epithelial cells in the pancreas that secretes pancreatic juice in the pancreas
alimentary canal
continuous muscular digestive tube that extends from the mouth to the anus
aminopeptidase
brush border enzyme that acts on proteins
anal canal
final segment of the large intestine
anal column
long fold of mucosa in the anal canal
anal sinus
recess between anal columns
appendix
(vermiform appendix) coiled tube attached to the cecum
ascending colon
first region of the colon
bacterial flora
bacteria in the large intestine
bile
alkaline solution produced by the liver and important for the emulsification of lipids
bile canaliculus
small duct between hepatocytes that collects bile
bilirubin
main bile pigment, which is responsible for the brown color of feces
body
mid-portion of the stomach
bolus
mass of chewed food
brush border
fuzzy appearance of the small intestinal mucosa created by microvilli
cardia
(also, cardiac region) part of the stomach surrounding the cardiac orifice (esophageal hiatus)
cecum
pouch forming the beginning of the large intestine
cementum
bone-like tissue covering the root of a tooth
central vein
vein that receives blood from hepatic sinusoids
cephalic phase
(also, reflex phase) initial phase of gastric secretion that occurs before food enters the stomach
chemical digestion
enzymatic breakdown of food
chief cell
gastric gland cell that secretes pepsinogen
chylomicron
large lipid-transport compound made up of triglycerides, phospholipids, cholesterol, and proteins
chyme
soupy liquid created when food is mixed with digestive juices
circular fold
(also, plica circulare) deep fold in the mucosa and submucosa of the small intestine
colon
part of the large intestine between the cecum and the rectum
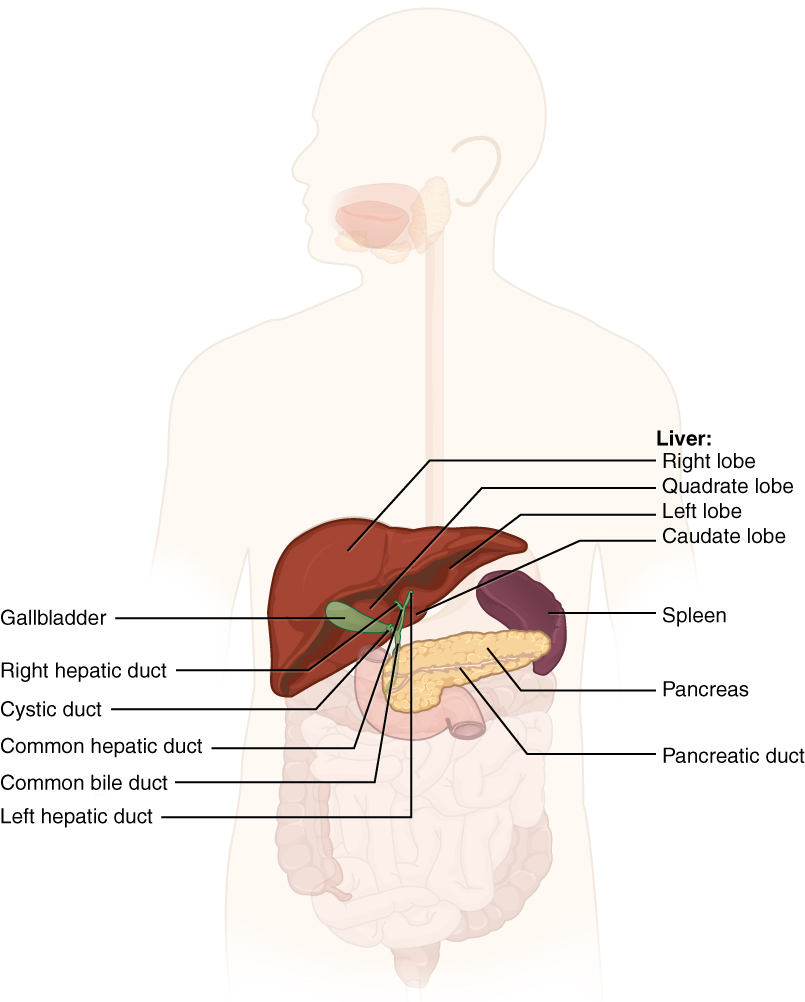
common bile duct
structure formed by the union of the common hepatic duct and the gallbladder’s cystic duct
common hepatic duct
duct formed by the merger of the two hepatic ducts
crown
portion of tooth visible superior to the gum line
cuspid
(also, canine) pointed tooth used for tearing and shredding food
cystic duct
duct through which bile drains and enters the gallbladder
deciduous tooth
one of 20 “baby teeth”
defecation
elimination of undigested substances from the body in the form of feces
deglutition
three-stage process of swallowing
dens
tooth
dentin
bone-like tissue immediately deep to the enamel of the crown or cementum of the root of a tooth
dentition
set of teeth
deoxyribonuclease
pancreatic enzyme that digests DNA
descending colon
part of the colon between the transverse colon and the sigmoid colon
dipeptidase
brush border enzyme that acts on proteins
duodenal gland
(also, Brunner’s gland) mucous-secreting gland in the duodenal submucosa
duodenum
first part of the small intestine, which starts at the pyloric sphincter and ends at the jejunum
enamel
covering of the dentin of the crown of a tooth
enteroendocrine cell
gastric gland cell that releases hormones
enterohepatic circulation
recycling mechanism that conserves bile salts
enteropeptidase
intestinal brush-border enzyme that activates trypsinogen to trypsin
epiploic appendage
small sac of fat-filled visceral peritoneum attached to teniae coli
esophagus
muscular tube that runs from the pharynx to the stomach
external anal sphincter
voluntary skeletal muscle sphincter in the anal canal
fauces
opening between the oral cavity and the oropharynx
feces
semisolid waste product of digestion
flatus
gas in the intestine
fundus
dome-shaped region of the stomach above and to the left of the cardia
G cell
gastrin-secreting enteroendocrine cell
gallbladder
accessory digestive organ that stores and concentrates bile
gastric emptying
process by which mixing waves gradually cause the release of chyme into the duodenum
gastric gland
gland in the stomach mucosal epithelium that produces gastric juice
gastric phase
phase of gastric secretion that begins when food enters the stomach
gastric pit
narrow channel formed by the epithelial lining of the stomach mucosa
gastrin
peptide hormone that stimulates secretion of hydrochloric acid and gut motility
gastrocolic reflex
propulsive movement in the colon activated by the presence of food in the stomach
gastroileal reflex
long reflex that increases the strength of segmentation in the ileum
gingiva
gum
haustral contraction
slow segmentation in the large intestine
haustrum
small pouch in the colon created by tonic contractions of teniae coli
hepatic artery
artery that supplies oxygenated blood to the liver
hepatic lobule
hexagonal-shaped structure composed of hepatocytes that radiate outward from a central vein
hepatic portal vein
vein that supplies deoxygenated nutrient-rich blood to the liver
hepatic sinusoid
blood capillaries between rows of hepatocytes that receive blood from the hepatic portal vein and the branches of the hepatic artery
hepatic vein
vein that drains into the inferior vena cava
hepatocytes
major functional cells of the liver
hepatopancreatic ampulla
(also, ampulla of Vater) bulb-like point in the wall of the duodenum where the bile duct and main pancreatic duct unite
hepatopancreatic sphincter
(also, sphincter of Oddi) sphincter regulating the flow of bile and pancreatic juice into the duodenum
hydrochloric acid (HCl)
digestive acid secreted by parietal cells in the stomach
ileocecal sphincter
sphincter located where the small intestine joins with the large intestine
ileum
end of the small intestine between the jejunum and the large intestine
incisor
midline, chisel-shaped tooth used for cutting into food
ingestion
taking food into the GI tract through the mouth
internal anal sphincter
involuntary smooth muscle sphincter in the anal canal
intestinal gland
(also, crypt of Lieberkühn) gland in the small intestinal mucosa that secretes intestinal juice
intestinal juice
mixture of water and mucus that helps absorb nutrients from chyme
intestinal phase
phase of gastric secretion that begins when chyme enters the intestine
intrinsic factor
glycoprotein required for vitamin B12 absorption in the small intestine
jejunum
middle part of the small intestine between the duodenum and the ileum
labial frenulum
midline mucous membrane fold that attaches the inner surface of the lips to the gums
labium
lip
lactase
brush border enzyme that breaks down lactose into glucose and galactose
lacteal
lymphatic capillary in the villi
large intestine
terminal portion of the alimentary canal
laryngopharynx
part of the pharynx that functions in respiration and digestion
left colic flexure
(also, splenic flexure) point where the transverse colon curves below the inferior end of the spleen
lingual frenulum
mucous membrane fold that attaches the bottom of the tongue to the floor of the mouth
lingual lipase
digestive enzyme from glands in the tongue that acts on triglycerides
lipoprotein lipase
enzyme that breaks down triglycerides in chylomicrons into fatty acids and monoglycerides
liver
largest gland in the body whose main digestive function is the production of bile
lower esophageal sphincter
smooth muscle sphincter that regulates food movement from the esophagus to the stomach
main pancreatic duct
(also, duct of Wirsung) duct through which pancreatic juice drains from the pancreas
major duodenal papilla
point at which the hepatopancreatic ampulla opens into the duodenum
maltase
brush border enzyme that breaks down maltose and maltotriose into two and three molecules of glucose, respectively
mass movement
long, slow, peristaltic wave in the large intestine
mastication
chewing
mechanical digestion
chewing, mixing, and segmentation that prepares food for chemical digestion
mesoappendix
mesentery of the appendix
micelle
tiny lipid-transport compound composed of bile salts and phospholipids with a fatty acid and monoacylglyceride core
microvillus
small projection of the plasma membrane of the absorptive cells of the small intestinal mucosa
migrating motility complex
form of peristalsis in the small intestine
mixing wave
unique type of peristalsis that occurs in the stomach
molar
tooth used for crushing and grinding food
motilin
hormone that initiates migrating motility complexes
motility
movement of food through the GI tract
mucosa
innermost lining of the alimentary canal
mucosal barrier
protective barrier that prevents gastric juice from destroying the stomach itself
mucous neck cell
gastric gland cell that secretes a uniquely acidic mucus
muscularis
muscle (skeletal or smooth) layer of the alimentary canal wall
myenteric plexus
(plexus of Auerbach) major nerve supply to alimentary canal wall; controls motility
nucleosidase
brush border enzyme that digests nucleotides
oral cavity
(also, buccal cavity) mouth
oral vestibule
part of the mouth bounded externally by the cheeks and lips, and internally by the gums and teeth
oropharynx
part of the pharynx continuous with the oral cavity that functions in respiration and digestion
palatoglossal arch
muscular fold that extends from the lateral side of the soft palate to the base of the tongue
palatopharyngeal arch
muscular fold that extends from the lateral side of the soft palate to the side of the pharynx
pancreas
accessory digestive organ that secretes pancreatic juice
pancreatic amylase
enzyme secreted by the pancreas that completes the chemical digestion of carbohydrates in the small intestine
pancreatic juice
secretion of the pancreas containing digestive enzymes and bicarbonate
pancreatic lipase
enzyme secreted by the pancreas that participates in lipid digestion
pancreatic nuclease
enzyme secreted by the pancreas that participates in nucleic acid digestion
parietal cell
gastric gland cell that secretes hydrochloric acid and intrinsic factor
parotid gland
one of a pair of major salivary glands located inferior and anterior to the ears
pectinate line
horizontal line that runs like a ring, perpendicular to the inferior margins of the anal sinuses
pepsinogen
inactive form of pepsin
peristalsis
muscular contractions and relaxations that propel food through the GI tract
permanent tooth
one of 32 adult teeth
pharynx
throat
phosphatase
brush border enzyme that digests nucleotides
porta hepatis
“gateway to the liver” where the hepatic artery and hepatic portal vein enter the liver
portal triad
bile duct, hepatic artery branch, and hepatic portal vein branch
premolar
(also, bicuspid) transitional tooth used for mastication, crushing, and grinding food
propulsion
voluntary process of swallowing and the involuntary process of peristalsis that moves food through the digestive tract
pulp cavity
deepest portion of a tooth, containing nerve endings and blood vessels
pyloric antrum
wider, more superior part of the pylorus
pyloric canal
narrow, more inferior part of the pylorus
pyloric sphincter
sphincter that controls stomach emptying
pylorus
lower, funnel-shaped part of the stomach that is continuous with the duodenum
rectal valve
one of three transverse folds in the rectum where feces is separated from flatus
rectum
part of the large intestine between the sigmoid colon and anal canal
reticuloendothelial cell
(also, Kupffer cell) phagocyte in hepatic sinusoids that filters out material from venous blood from the alimentary canal
retroperitoneal
located posterior to the peritoneum
ribonuclease
pancreatic enzyme that digests RNA
right colic flexure
(also, hepatic flexure) point, at the inferior surface of the liver, where the ascending colon turns abruptly to the left
root
portion of a tooth embedded in the alveolar processes beneath the gum line
ruga
fold of alimentary canal mucosa and submucosa in the empty stomach and other organs
saccharolytic fermentation
anaerobic decomposition of carbohydrates
saliva
aqueous solution of proteins and ions secreted into the mouth by the salivary glands
salivary amylase
digestive enzyme in saliva that acts on starch
salivary gland
an exocrine gland that secretes a digestive fluid called saliva
salivation
secretion of saliva
segmentation
alternating contractions and relaxations of non-adjacent segments of the intestine that move food forward and backward, breaking it apart and mixing it with digestive juices
serosa
outermost layer of the alimentary canal wall present in regions within the abdominal cavity
sigmoid colon
end portion of the colon, which terminates at the rectum
small intestine
section of the alimentary canal where most digestion and absorption occurs
soft palate
posterior region of the bottom portion of the nasal cavity that consists of skeletal muscle
stomach
alimentary canal organ that contributes to chemical and mechanical digestion of food from the esophagus before releasing it, as chyme, to the small intestine
sublingual gland
one of a pair of major salivary glands located beneath the tongue
submandibular gland
one of a pair of major salivary glands located in the floor of the mouth
submucosa
layer of dense connective tissue in the alimentary canal wall that binds the overlying mucosa to the underlying muscularis
submucosal plexus
(plexus of Meissner) nerve supply that regulates activity of glands and smooth muscle
sucrase
brush border enzyme that breaks down sucrose into glucose and fructose
tenia coli
one of three smooth muscle bands that make up the longitudinal muscle layer of the muscularis in all of the large intestine except the terminal end
tongue
accessory digestive organ of the mouth, the bulk of which is composed of skeletal muscle
transverse colon
part of the colon between the ascending colon and the descending colon
upper esophageal sphincter
skeletal muscle sphincter that regulates food movement from the pharynx to the esophagus
Valsalva’s maneuver
voluntary contraction of the diaphragm and abdominal wall muscles and closing of the glottis, which increases intra-abdominal pressure and facilitates defecation
villus
projection of the mucosa of the small intestine
voluntary phase
initial phase of deglutition, in which the bolus moves from the mouth to the oropharynx
α-dextrin
breakdown product of starch
α-dextrinase
brush border enzyme that acts on α-dextrins
Dưới đây là các bài văn nằm ở bên trái. Ở bên phải là các bài luyện tập (practice) để đánh giá khả năng đọc hiểu của bạn. Sẽ khó khăn trong thời gian đầu nếu vốn từ vựng của bạn còn hạn chế, đặc biệt là từ vựng Y khoa. Hãy kiên nhẫn và đọc nhiều nhất có kể, lượng kiến thức tích tụ dần sẽ giúp bạn đọc thoải mái hơn.
Dưới đây là video và các luyện tập (practice) của bài này. Nghe là một kĩ năng khó, đặc biệt là khi chúng ta chưa quen nội dung và chưa có nhạy cảm ngôn ngữ. Nhưng cứ đi thật chậm và đừng bỏ cuộc.
Dưới đây là phần bàn luận. Bạn có thể tự do đặt câu hỏi, bổ sung kiến thức, và chia sẻ trải nghiệm của mình.
Subscribe
Login
0 Comments
Ấn vào ô bên dưới để đánh dấu bạn đã hoàn thành bài học này
Quá dữ! Tiếp tục duy trì phong độ nhé!